This Reading Room is a collaboration between MedPage Today® and:

For adrenal insufficiency (AI), reducing false positives means more than reducing resource utilization. Treatments like glucocorticoid replacement therapy can cause serious harm in people who do not actually have AI.
Research published in the Journal of the Endocrine Society makes multiple findings that report authors say could help bring down false positive rates for AI. This retrospective study ultimately analyzed 6,531 medical records from the Imperial College Healthcare NHS Trust in the United Kingdom.
Sirazum Choudhury, MBBS, an endocrinologist-researcher with the trust, served as a co-author of the report. He discussed the study with MedPage Today. The exchange has been edited for length and clarity.
This study ultimately addressed two related but distinct questions. What was the first?
Choudhury: Initially the path we were following had to do with when cortisol levels are tested.
Cortisol levels follow a diurnal pattern; levels are highest in the morning and then decline to almost nothing overnight. This means we ought to be measuring the level in the morning. But there are logistical issues to doing so. In many hospitals, we end up taking measurements of cortisol in the afternoon. That creates a dilemma, because if it comes back low, there's an issue as to what we ought to do with the result.
Here at Imperial, we call out results of <100 nmol/L among those taken in the afternoon. Patients and doctors then have to deal with these abnormal results, when in fact they may not actually be abnormal. We may be investigating individuals who should really not be investigated.
So the first aim of our study was to try and ascertain whether we could bring that down to a lower level and in doing so stop erroneously capturing people who are actually fine.
What was the second aim of the study?
Choudhury: As we went through tens of thousands of data sets, we realized we could answer more than that one simple question. So the next part of the study became: if an individual is identified as suspicious for AI, what's the best way to prove this diagnosis?
We do this with different tests like short Synacthen Tests (SST), all with different cutoff points. Obviously, we want to get the testing right, because if you falsely label a person as having AI, the upshot is that treatments will interfere with their cortisol access and they will not do well. Simply put, we would be shortening their life.
So, our second goal was to look at all the SSTs we've done at the center and track them to see whether we could do better with the benchmarks.
What did you find?
Choudhury: When you look at the data, you see that you can bring those benchmarks down and potentially create a more accurate test.
First, we can be quite sure that a patient who is tested in the afternoon and whose cortisol level is >234 does not have AI. If their level is <53.5 then further investigation is needed
There were similar findings for SSTs, which in our case were processed using a platform made by Abbott. For this platform, we concluded that the existing cut-offs should be dropped down to 367 at 30 minutes or 419 at about 60 minutes.
Did anything surprise you about the study or its findings?
Choudhury: If you look at the literature, the number of individuals who fail at 30 minutes but pass at 60 minutes is around 5%. But I was very surprised to see that our number at Imperial was about 20%.
This is a key issue because, as I mentioned, if individuals are wrongly labelled adrenally insufficient, you're shortening their life. It's scary to think about the number of people who might have been given steroids and treated for AI when they didn't have the condition.
What do you see as the next steps?
Choudhury: I see centers unifying their cutoffs for SST results and making sure we're all consistent in the way we treat these results.
From a research perspective, on the testing we're obviously talking about one specific platform with Abbott, so research needs to be done on SST analyzers from other manufacturers to work out what their specific cutoffs should be.
Read the study here and expert commentary on the clinical implications here.
The study authors did not disclose any relevant relationship with industry.
Primary Source
Journal of the Endocrine Society
From https://www.medpagetoday.com/reading-room/endocrine-society/adrenal-disorders/95661


























Desmopressin Stimulation Test in a Pregnant Patient with Cushing’s Disease
in News Items and Research
Posted
Highlights
Due to the physiologic rise of ACTH during pregnancy, unstimulated ACTH levels may not be an accurate marker to differentiate between adrenal and ACTH-independent Cushing's syndrome.
The desmopressin stimulation test can be done during pregnancy to investigate the etiology of Cushing's syndrome.
Non-gadolinium enhanced pituitary imaging may not detect pituitary adenoma, which is the most common cause of Cushing's disease. Contrast-enhanced pituitary magnetic resonance imaging should be considered in pregnant women with ACTH-dependent Cushing's syndrome.
Due to increase maternal and fetal morbidities in active Cushing's syndrome, prompt diagnosis and appropriate treatment are essential. The treatment of choice is transsphenoidal surgery during the second trimester, preferably at a high-volume pituitary center.
There were significantly lower rates of fetal complications in women with active Cushing's syndrome than a cured disease, including low birth weight.
Abstract
Objective
The hypothalamic-pituitary-adrenal axis stimulation during pregnancy complicates the investigation of Cushing's syndrome. Our objective is to present a pregnant patient with Cushing syndrome caused by pituitary tumor in which the desmopressin stimulation test helped in the diagnosis and led to appropriate management.
Case report
A 27-year-old woman with 9-week gestation presented with proximal myopathy for 2 months. She had high blood pressure, wide abdominal purplish striae, and proximal myopathy. Her past medical history revealed hypertension and dysglycemia for 1 year. The 8 AM cortisol was 32.4 μg/dL (5-18), late-night salivary cortisol at 11 PM was 0.7 μg/dL (<0.4), and the mean 24-hour urinary free cortisol was 237.6 μg/day (21.0-143.0). The mean ACTH concentrations at 8 AM were 44.0 pg/mL (0-46.0). Non-gadolinium enhanced pituitary magnetic resonance imaging (MRI) reported no obvious lesion. The desmopressin stimulation test showed a 70% increase in ACTH levels from baseline after desmopressin administration. The pituitary MRI with gadolinium showed an 8x8x7-mm pituitary adenoma. Transsphenoidal surgery with tumor removal was done, which showed ACTH-positive tumor cells. After the surgery, the patient carried on the pregnancy uneventfully.
Discussion
During pregnancy, the ACTH level may not be an accurate marker to help in the differential diagnosis of Cushing's syndrome. Moreover, non-gadolinium pituitary imaging may not detect small pituitary lesions.
Conclusion
In the present Case, the desmopressin stimulation test suggested the diagnosis of Cushing's disease, which subsequently led to successful treatment. This suggested that the desmopressin test may serve as a useful test to diagnose Cushing's disease in pregnant individuals.
Keywords
Introduction
Pregnancy rarely occurs during the course of Cushing's syndrome (CS).1,2 Given the increase in maternal and fetal morbidities in women with active CS, early diagnosis and treatment of CS are essential.2
The diagnosis of CS using the usual diagnostic tests is challenging due to stimulation of the hypothalamic-pituitary-adrenal axis during pregnancy. The physiologic rise of ACTH from the 7th week of pregnancy also complicates the investigation for the etiology of CS.1 The concern of gadolinium use during pregnancy can affect the sensitivity in detecting small pituitary lesions in ACTH-dependent CS if using non-gadolinium pituitary imaging. Desmopressin is a vasopressin analog selective for V2 receptors. The desmopressin stimulation test has been proposed as a useful procedure for the differential diagnosis of CS.3 Desmopressin stimulates the increase in ACTH and cortisol in patients with CS caused by pituitary tumor or Cushing's disease (CD) but not in the majority of normal, obese subjects and patients with adrenal CS or ectopic ACTH syndrome.3,4 However, there were limited data on the desmopressin stimulation test during pregnancy.
Here we present the 27-year-old woman with CS in which the desmopressin stimulation test helped in the diagnosis of CD and led to successful treatment.
Case presentation
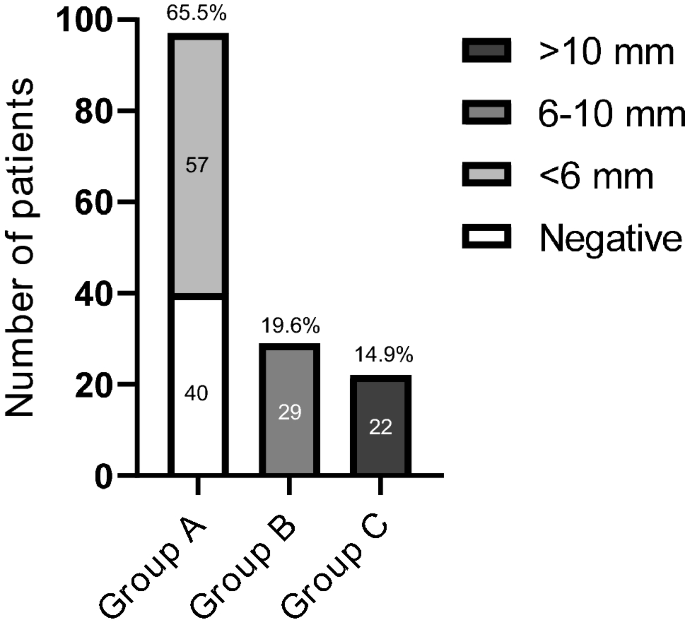
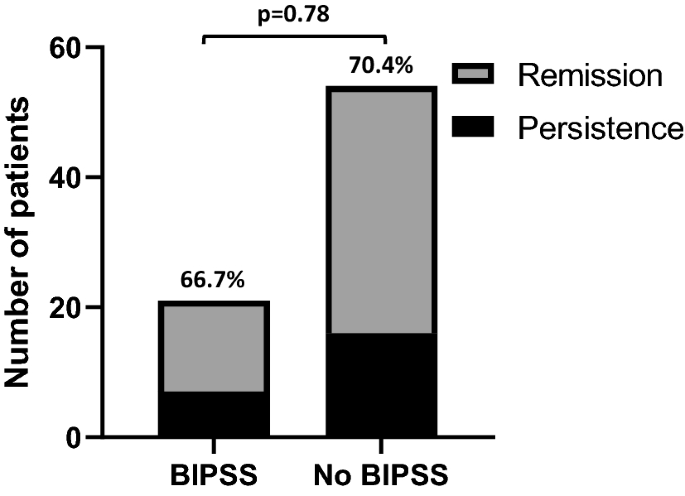
A 27-year-old woman with 9-week gestation was referred from the orthopedic department to evaluate CS. She presented with proximal myopathy for 2 months. On physical examination, she had Cushingoid appearance, wide purplish striae, bruising, and proximal muscle weakness. Her blood pressure was 160/100 mmHg, and her body mass index was 32.2 kg/m2. Her past medical history revealed that she had hypertension, dyslipidemia, and impaired fasting glucose for 1 year without taking any medication. She also gained 20 kg in the past 2 years. The 8 AM cortisol (chemiluminescent immunometric assay, Immulite/Siemens) was 32.4 μg/dL (normal , 5.0-18.0), late-night salivary cortisol at 11 PM (electrochemiluminescence immunoassay, Roche Cobas) was 0.7 μg/dL (normal, <0.4), and the mean 24-hour urinary free cortisol (UFC) (radioimmunoassay, Immulite/Siemens) was 237.6 μg/day (normal, 21.0-143.0). ACTH concentrations at 8 AM (chemiluminescent immunometric assay, Immulite/Siemens) were 48.4 and 39.6 pg/mL (normal, 0-46.0) (Table 1). At 12 weeks of gestation, non-gadolinium enhanced pituitary magnetic resonance imaging (MRI) reported a mild bulging contour of the right lateral aspect of the pituitary gland without an obvious abnormal lesion (Figure 2A). The desmopressin stimulation test was then carried out at 14 weeks of gestation. Serial blood samples for ACTH and cortisol were obtained basally (at 8 AM) and at 15, 30, 45, and 60 minutes after the intravenous administration of 10 μg of desmopressin. The results were shown in Table 2. Compared with baseline, ACTH levels increased from 34.7 to 58.9 pg/mL (70%) at 15 minutes after desmopressin administration (a ≥35% increase in ACTH levels was considered an indication of CD in non-pregnant individuals)3 (Figure 1). The pituitary MRI with gadolinium revealed an 8x8x7-mm circumscribed lesion with heterogeneous iso- to hyperintensity on T2W in the right inferolateral aspect of the anterior pituitary lobe. The lesion had a delayed enhancement compared to normal pituitary tissue (Figure 2B). Non-contrast MRI adrenal glands showed bilateral normal adrenal glands without mass or nodule. Other abdominal organs were unremarkable. Regarding comorbidities, she had hypertension and gestational diabetes mellitus (GDM). The HbA1c level was 5.7% (39 mmol/mol). Using a two-step strategy, GDM was diagnosed at 12 weeks of gestation. Hypertension and GDM were controlled with 750 mg of methyldopa and 50 units of insulin per day, respectively.
Table 1. Laboratory investigations of the present Case
UFC, urinary free cortisol; ACTH, adrenocorticotrophic hormone; DHEAS, dehydroepiandrosterone sulphate; PAC, plasma aldosterone concentration; PRA, plasma renin activity.
Figure 2. Pituitary imaging of the present Case. (A) A non-gadolinium MRI of the pituitary gland at 12 weeks of gestation showing a mild bulging contour of the right lateral aspect of the pituitary gland without an obvious abnormal lesion (B) An MRI of the pituitary gland with gadolinium at 14 weeks of gestation showing an 8x8x7-mm circumscribed lesion with heterogeneous iso- to hyperintensity on T2W in the right inferolateral aspect of the anterior pituitary lobe. The lesion had a delayed enhancement compared to normal pituitary tissue.
Table 2. Desmopressin stimulation test results performing at 14 weeks of gestation
ACTH, adrenocorticotrophic hormone
Figure 1. Percentage of ACTH increase after desmopressin administration (time 0 min).
Transsphenoidal surgery with tumor removal was performed at 18 weeks of gestation. Pathological findings showed a 1.3x1.0x0.3 cm of tissue with segments of the pituitary gland and tumor. There were monomorphous round nuclei, stippled chromatin, indistinct nucleoli, and pale eosinophilic cytoplasm cells. These cells were reactive with ACTH and showed loss of reticulin framework, unlike the normal pituitary gland. The next day after the surgery, her 8 AM cortisol was 6.0 μg/dL. Hydrocortisone supplement was started and continued throughout pregnancy. Antihypertensives were discontinued, and the insulin dosages decreased to less than 20 units per day. At 38 weeks of gestation, she gave birth to a 2300-gm male newborn (small for gestational age). Dysglycemia and hypertension resolved after the delivery. One year after the first child's delivery, the patient had a spontaneous pregnancy without GDM or hypertension. The 8 AM cortisol was 3.9 μg/dL, and hydrocortisone replacement was continued. The patient successfully delivered a term 3300-gm male infant without fetal or maternal complications. Two years after the first transsphenoidal surgery, a 1-μg cosyntropin stimulation test was performed, the basal cortisol was 11.7 μg/dL, and the peak serum cortisol was 23.8 μg/dL. Steroid replacement was withdrawn.
Discussion
Herein we present a 27-year-old woman who was evaluated during her first pregnancy for clinical and laboratory features suggestive of CD. Her morning serum and late-night salivary cortisol concentrations were elevated in addition to non-suppressed ACTH, but a definitive diagnosis was not obtained by a non-gadolinium pituitary MRI. The diagnosis of CD was suggested, however, by the results of a desmopressin stimulation test. The pituitary MRI with gadolinium was proceeded and revealed a pituitary lesion greater than 6 mm.
The prevalence of pregnancy is low due to reduced fertility in CS. To date, there have been less than 300 pregnant patients with CS reported in the literature.2 In pregnancy, the most frequent etiology of CS is adrenal CS (60%), followed by ACTH-producing pituitary adenomas or CD (35%), and very rarely ectopic ACTH (<5%).1 In contrast, CD is the most common cause of CS in non-pregnant people (approximately 70 percent). The clinical diagnosis of CS during pregnancy may be missed due to overlapping features between pregnancy and CS. However, wide purplish cutaneous striae and proximal myopathy are signs with high discrimination index when CS is suspected.5 These signs are not present in normal pregnancy.
In this present Case, CS was diagnosed with apparent clinical features of CS in addition to an elevated UFC and late-night salivary cortisol. The patient denied taking any supplements and her 8 AM cortisol was not suppressed and therefore did not suggest an etiology of exogenous steroid use. Pregnant women without CS may have elevated UFC and late-night salivary cortisol due to increased total and free plasma cortisol from the first trimester until the end of pregnancy.6 This results from an elevated concentration of cortisol transport protein and the increase in placental ACTH and CRH. According to the current guideline, UFC is the recommended test when CS is suspected during pregnancy.5 Since UFC increases during the second trimester, it may not be a reliable marker after the first trimester of pregnancy unless the level is clearly increased (up to 2- to 3-fold the upper limit of normal values).1 Late-night salivary cortisol is also one of the useful tests to diagnose CS during pregnancy because the circadian rhythm of cortisol is preserved in normal pregnancy. Furthermore, it is not influenced by the changes in the binding proteins.7 However, the previous study has shown that late-night salivary cortisol increased progressively throughout pregnancy. When compared with non-pregnant women, median values of late-night salivary cortisol in pregnant women were 1.1, 1.4, and 2.1 times higher in the first, second, and third trimesters respectively. The cutoff values for late-night salivary cortisol on each gestational trimester were: first trimester 0.255 μg/dL, second trimester 0.260 μg/dL, and third trimester 0.285 μg/dL. The respective sensitivities and specificities in each trimester were: first trimester 92 and 100%, second trimester 84 and 98%, and third trimester 80 and 93%.8
Given the non-suppressed ACTH levels after the 7th week of gestation, we were not able to summarize whether the etiology was adrenal CS or ACTH-dependent CS which could be either CD or ectopic ACTH syndrome. In non-pregnant individuals, ACTH suppression usually identifies adrenal CS. However, in pregnancy, ACTH levels were non-suppressed in half of those with adrenal CS due to continued stimulation of maternal hypothalamic-pituitary-adrenal axis by placental CRH.1 Therefore, using the ACTH thresholds in general populations can lead to misdiagnosis when investigating the etiology of CS in pregnant individuals. The hypothalamic-pituitary-adrenal axis response to exogenous glucocorticoids is blunted in pregnant women. Following an overnight dexamethasone administration, pregnant women without CS may have non-suppressed plasma cortisol and UFC.6 In non-pregnant individuals with CS, the high-dose dexamethasone suppression test identify CD with a sensitivity of 82% and a specificity of 50%.4 During pregnancy, the high-dose dexamethasone suppression test failed to identify almost half of the patients with CD.1 Inferior petrosal sinus sampling is usually avoided due to the risk of excessive radiation exposure. Since the non-gadolinium MRI also showed no obvious pituitary lesion in the present Case, in addition to the limitation of the high-dose dexamethasone suppression test and inferior petrosal sinus sampling in pregnancy, we used desmopressin stimulation to help in the investigation of CD since desmopressin can stimulate an ACTH response in a considerable proportion of patients with CD but not in most patients with adrenal CS or ectopic ACTH syndrome.3,4
Desmopressin has been assigned to pregnancy category B by the US Food and Drug Administration (FDA). In the most recent guideline update on the diagnosis and management of CD, the desmopressin stimulation test can be used to differentiate ectopic CS and CD in patients with normal or high ACTH and have no adenoma or equivocal results of pituitary MRI. However, the guideline did not mention the use of this test in pregnant individuals.9 The literature regarding the use of desmopressin stimulation tests in pregnancy is limited. We were able to identify one study in a pregnant patient with active CS, who was surgically confirmed as CD, in which the desmopressin stimulation test was performed at 10 weeks of gestation and after the delivery. Compared with age-matched healthy non-pregnant women, there were different responses of cortisol and ACTH after desmopressin administration in a pregnant patient with active CS.10 The ACTH peaks after the administration of desmopressin were higher in the pregnant patient. CRH stimulation test was also performed in the pregnant patient with CD. Desmopressin stimulated ACTH values during pregnancy and after the delivery were not significantly different, while the CRH stimulated ACTH values were significantly higher when the test was performed after the delivery. The authors did not mention optimal cutoff values for these diagnostic tests.10 In non-pregnant individuals, the ACTH increase of more than 35% at 15 minutes after the desmopressin administration gave the sensitivity of 84% and the specificity of 43% in the diagnosis of CD.3 Another recent study in ACTH-dependent CS showed that the threshold increase in the ACTH level after desmopressin stimulation of 45% identified CD with a sensitivity of 91% and a specificity of 75%.4 Using the non-pregnant cutoff values for the desmopressin stimulation test, the diagnosis of CD was made in our patient who was later surgically confirmed as CD.
Pituitary microadenomas were the cause of CD in almost 90% of non-pregnant individuals.11 In pregnant women with CD, pituitary microadenomas were also reported to be more common than macroadenomas.1,12 Almost 40% of pituitary microadenomas in CD were invisible or poorly visible in non-contrast MRI, in which contrast-enhanced MRI detected them.13 In the Case series from Lindsay et al., the non-contrast MRI could not correctly identify pituitary adenomas in 38% of pregnant patients with available data.1 The same case series reported a pregnant patient having normal pituitary MRI and was later surgically confirmed as having CD from a 3x3 adenoma with positive staining for ACTH. In the present case, a mild bulging contour of the pituitary gland, although without an obvious abnormal lesion, in addition to desmopressin test results, suggested the need for contrast-enhanced pituitary MRI. Gadolinium contrast is FDA pregnancy category C since it is water-soluble and can cross the placenta into the fetus and amniotic fluid.14 However, since a non-gadolinium MRI may not detect pituitary microadenoma even in patients with normal imaging results,1,15 we suggested physicians consider pituitary MRI with gadolinium as initial imaging in pregnant patients with clinical suspicion of CD.
Prompt diagnosis and treatment of CS are essential due to a higher rate of fetal loss in active CS patients without treatment than those who received either medical or surgical treatment. There are significantly lower rates of various fetal complications, including low birth weight, in women with active CS than in cured CS.2 Although medical and surgical treatment were not compared as prognostic factors for complications, experts recommend transsphenoidal surgery in the second trimester as the treatment of choice for CD in pregnancy.1,15 Medical treatment should be the second choice when surgery cannot be carried out or late diagnosis is made.
Conclusion
In the present Case, the results from the desmopressin stimulation test and the pituitary MRI with gadolinium suggested the diagnosis of CD, which subsequently led to successful treatment. This suggested that the desmopressin test may serve as a useful test to diagnose CD even in the context of pregnancy.
Conflicts of Interest
None of the authors have any potential conflicts of interest associated with this research.
References
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
The authors would like to thank you all the colleagues in the Division of Endocrinology and Metabolism, Department of Medicine, Faculty of medicine, Chulalongkorn University for all the support.